- Why Vim Why Vim
-
Solutions
Solutions
-
Value-Based Care
Explore Vim’s value-based care solutions.
-
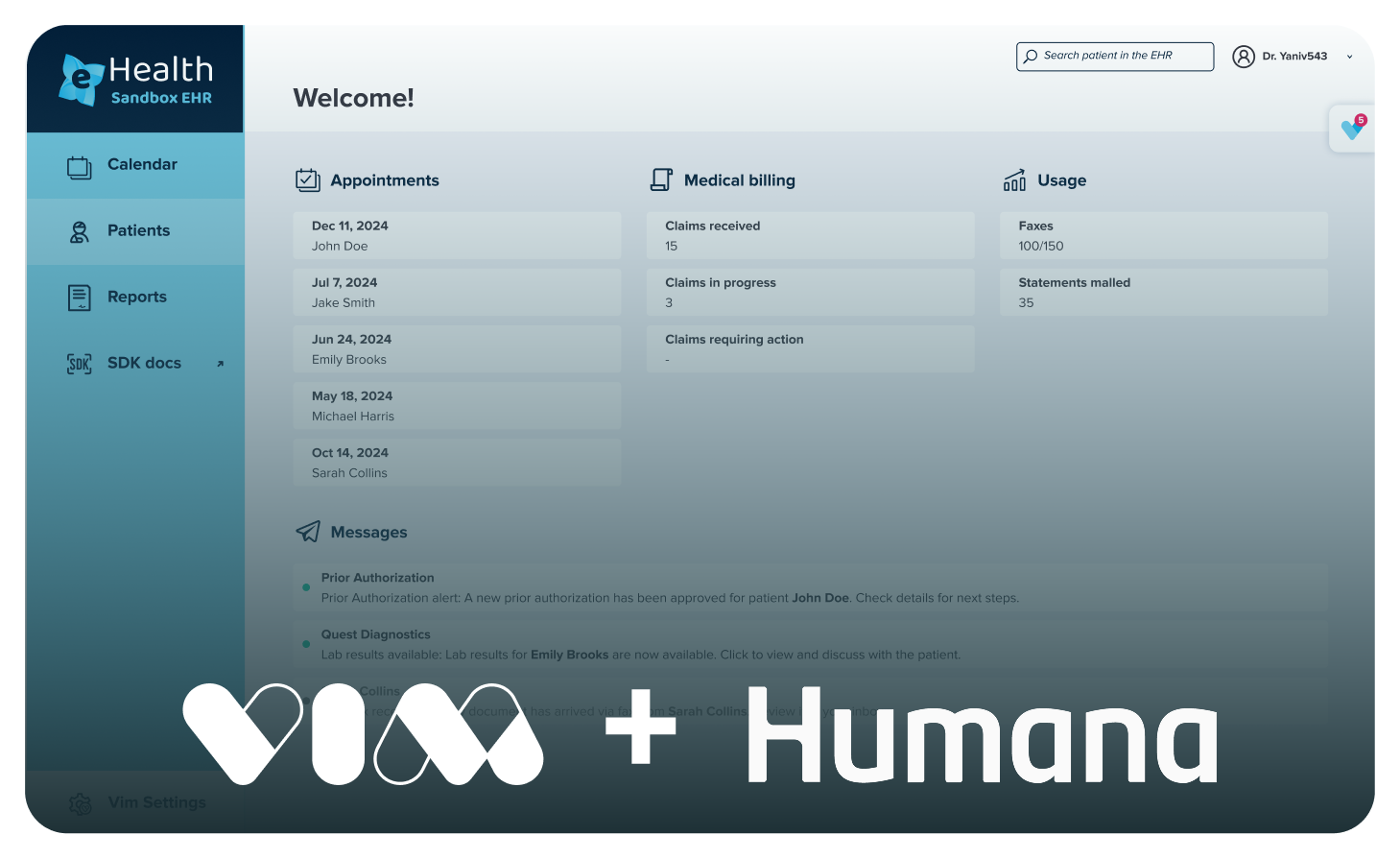
Vim Connect
Bring your healthcare app to life.
-
Marketplace
Discover the possibilities with our app marketplace.
Vim’s solutions connect stakeholders across healthcare in one powerful platform -
Value-Based Care
-
For Your Organization
For Your Organization-
Provider Networks
Explore Vim for providers.
-
Payers
Explore Vim for payers.
-
EHRs
Explore Vim for EHRs.
-
Health Tech Innovators
Explore Vim for health tech innovators.
Whether you’re a payer, provider, EHR, or developer, Vim delivers the tools to drive performance. -
Provider Networks
- Outcomes Outcomes
- Resources Resources
-
Company
Company